In terms of his psychiatric history, Mr. C first began to experience auditory and visual hallucinations at age 48, as well as a decline in cognition that led to his retirement from employment shortly thereafter. He has had 3 inpatient psychiatric admissions, and has continued to be treated with antipsychotics as discontinuation often leads to relapse of his psychosis.
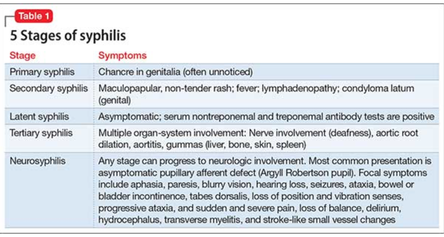
While Mr. C has a history of aortic regurgitation, CHF, HTN, and sensorineural hearing loss, he also describes a history of cocaine abuse from 21-45. More interestingly, he also reveals a diagnosis of syphilis at 48yo, which went untreated for many months until he was diagnosed with neurosyphilis (tertiary syphilis) after developing abnormal gait, blurred vision, and general weakness.
Do you think Mr. C's psychiatric symptoms are related to his diagnosis of neurosyphilis? What tests would you order? What would you advise him on further management/treatment?
"Psychosis in Treated Neurosyphilis: Is Now The Time To Stop His Antipsychotic?" by Kamalika Roy, Richard Balon, and Varma Penumetcha.








 RSS Feed
RSS Feed
