Can you come up with a diagnosis or treatment plan?
"He's been making new 'friends'" by Kamal Bhatia, Sneha Jadhav, and Amad Din (Current Psychiatry).
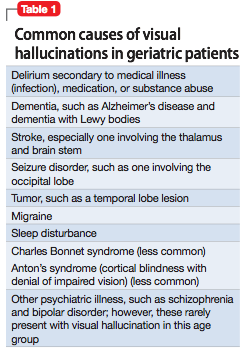
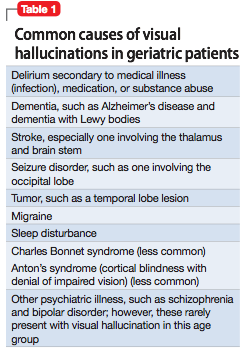 Put your knowledge and skills to the test with the case of a 91 year old man who presents to the ER for hip pain. During his visit, the patient describes to staff seeing "friends" who talk to him, and also sing and dance for him. These visual hallucinations have been ongoing for the last 4-5 months. The patient does not endorse any other psychiatric symptoms, and says he knows that these people are likely not real nor are they distressing to him, but they do keep him company. Can you come up with a diagnosis or treatment plan? "He's been making new 'friends'" by Kamal Bhatia, Sneha Jadhav, and Amad Din (Current Psychiatry).
0 Comments
 In this must read three part series (links below), The Boston Globe provides an in-depth look at mental illness as readers meet Michael Bourne, a 33 year old man with a long history of mental health issues, as well as his loving mother Peggy Bourne who throughout the years still tirelessly continues to be his support and caregiver. In this powerful series, one gets a unique and important perspective, as you hear about a family desperately trying to navigate the mental health system and trying to accomplish the challenging task of getting their loved one proper treatment and keeping them safe and in recovery for more than a few weeks or months at a time ... it's a story that is all too common. "Mike was 33 years old. He’d been in and out of institutions for half his life, since he first got sick when he was 17. His diagnosis had changed over the years — it was #schizophrenia, then #bipolar disorder, then #schizoaffective disorder — and his medications were in constant flux. Things stayed good for a while, then went bad again. Now Mike’s medications seemed to be working, and he was saying that he wanted to stay on them — a view he didn’t always take. But there had been so many days like this, so many hopeful new beginnings. Often, when bringing him home from a hospital stay, Peggy saw again the man she knew: funny and charming, intelligent and sweet. And then she watched that man disappear, receding from her as though into the depths of a lake. He was replaced by someone else, whose thoughts she did not understand. Mike suffered at times from #delusions. His mother never feared him, but some of the neighbors did, interpreting his loudness and profanity as threatening. Peggy had lived for years with the constant worry. She had lived with the complaints from neighbors and the calls from the police in the middle of the night; she had coped with Mike giving all his money to strangers or throwing all their food away, believing it was poisoned. She had watched his friends grow up and get jobs and get married, while he remained trapped in place. Yet she still believed that one day, the right treatment would free them. Mike would stay well, and she would have her son back."
 Put your knowledge and skills to the test with the case of a 19 year old man who presents with anxiety, agitation, isolation, social withdrawal, and paranoia. He is determined by the healthcare team to be experiencing his first psychotic break, is given the diagnosis of psychosis - not otherwise specified, and is treated first with risperidone and then haloperidol. A year later, the patient presents again to hospital with the same symptoms (as above), as well as a recent history of alcohol abuse. Several medications are tried, but his symptoms persist and he remains unable to resume his normal activities. Eventually, he is prescribed clozapine, an atypical antipsychotic approved for use in treatment-resistant schizophrenia. This new medication helps to relieve his psychotic symptoms, but his heart rate is persistently elevated. Can you determine the cause of this patient's tachycardia or come up with a management plan? "A young man with psychosis whose heart is racing" by Kim Brownell, Dana Sinopoli, Karlyn Huddy, and Amy Taylor (Current Psychiatry) 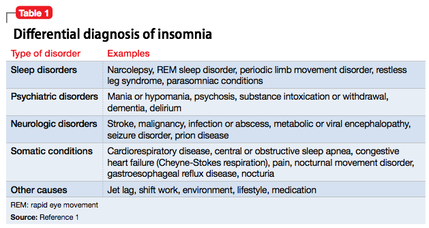 Put your knowledge and skills to the test with the case of a 44 year old male who presents with disorientation, impaired attention and concentration, paranoid delusions, and auditory and visual hallucinations, all of which began 6 months ago when his sleep began to deteriorate. He has had a history of depression following his brother's death from an unknown neurologic disease 3 years ago, and has been using marijuana daily for a number of years. Can you determine the cause of his insomnia and symptoms or come up with a treatment plan? "Sleepless and Paranoid" by Nick Eilbeck & Marijo Tamburrino (Current Psychiatry) 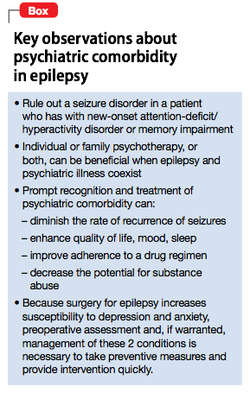 It is not uncommon for patients to have multiple comorbidities, including those that are physical as well as mental in origin. As most of us would guess, one illness can often have an impact on other aspects of a patient's life, including making management of other medical conditions more complex, and increasing the risk of developing further health issues. This sort of relationship has been seen between seizure disorders like #epilepsy and psychiatric disorders. In the resource, "Managing Psychiatric Illness in Patients With Epilepsy" by Sowmya C. Puvvada, Satyanarayana Kommisetti, & Abhishek Reddy, readers can learn how to distinguish between features of epilepsy and signs/symptoms of common mental health conditions (such as substance abuse disorders, sleep disorders, and anxiety), discover the links between seizures and mental illness, and learn the preferred management and treatment strategies for depression and psychosis among those with seizure disorders along with gaining other clinical pearls. "Patients who have epilepsy have a higher incidence of psychiatric illness than the general population—at a prevalence of 60%. Establishing a temporal association and making a psychiatric diagnosis can be vexing, but awareness of potential comorbidities does improve the clinical outcome. As this article discusses, psychiatric presentations and ictal disorders can share common pathology and exacerbate one another. Their coexistence often results in frequent hospitalization, higher treatment cost, and drug-resistant seizures. Risk factors for psychopathology in people who have epilepsy include psychosocial stressors, genetic factors, early age of onset of seizures, and each ictal event. Among ictal disorders, temporal-lobe epilepsy confers the highest rate of comorbidity" (Current Psychiatry).  "What Michael Did" is a powerful and moving story about Michael Stewart, a Canadian man with schizophrenia, who back in 2002 when he was just 23 killed his mother during a psychotic episode. In the article, readers are given an intimate look into one family's experience with schizophrenia, as well as the confusing and scary time in which they witnessed the smart and witty Michael they used to know transform into someone else almost entirely ... someone who was paranoid, agitated, lost, and suffering from delusions and hallucinations, including believing that others could read his mind. Though a heartbreaking tragedy, the story manages to also be inspiring by demonstrating the immense resilience of the Stewart family, and shedding light into how they coped with the loss of one family member and forgiving another who had committed the act. A must read! 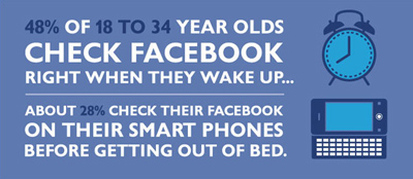 Put your knowledge and skills to the test with the case of a patient who is "obsessed with Facebook" and is becoming noticeably paranoid and agitated by posts made by his friends and sibling. The patient also has a history of depression, ADHD, and anger management issues. Can you make the diagnosis or come up with a treatment plan? How does social media play a role in mental health and what recommendations can be given to patients in how to prevent "facebook-induced distress"? "Obsessed With Facebook" by Jonathan R. Dattilo, Stephen P. Juraschek, and Anita Everett (Current Psychiatry) |
Description
Supporting and enhancing students' and health professionals' knowledge and understanding of mental health and psychiatry
Archives
June 2017
Categories
All
|