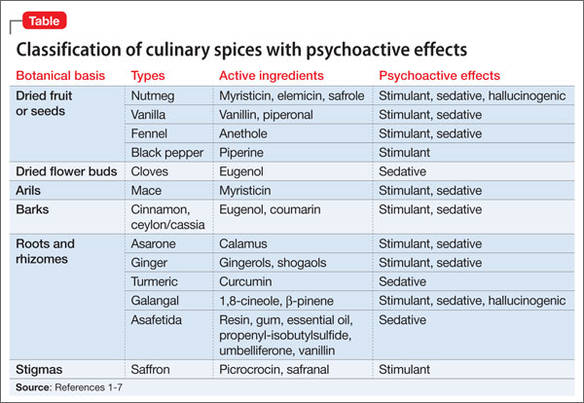
While spices may not be commonly abused substances, they are legal, readily available, and are ideal recreational substances for those including youth, those in the prison system or even those who are under drug monitoring and are looking for a "legal high" as these spices cannot be identified with toxicology testing.
"Clinicians often are unaware of a patient’s misuse or abuse of easily accessible substances such as spices, herbs, and natural supplements. This can lead to misdiagnosed severe psychiatric disorders and, more alarmingly, unnecessary use of long-term psychotropics and psychiatric services...
Acute nutmeg intoxication [for example] produces anxiety, fear, and hallucinations, and generally is self-limited, with most symptoms resolving within 24 hours. Chronic effects of nutmeg abuse resemble those of marijuana abuse."
To learn more about abuse of spices and their psychoactive effects, check out these two articles:
- "Out of the cupboard and into the clinic: Nutmeg-induced mood disorder" by Parthasarathi U, Hategan A and Bourgeois JA (Current Psychiatry).
- "Taking the spice route: Psychoactive properties of culinary spices" by Bourgeois JA, Parthasarathi U, and Hategan A (Current Psychiatry).






 RSS Feed
RSS Feed
