.
In this video, we see examples to help us navigate between different thought forms including circumstantial, tangential, loose associations and flight of ideas.
|
Feeling like practicing some of your mental status examination skills? Determining a patient's "thought process" can be tricky, but having this skill can prove helpful in terms of earlier recognition of mental health conditions such as mania . In this video, we see examples to help us navigate between different thought forms including circumstantial, tangential, loose associations and flight of ideas.
0 Comments
 Sally Buchanan-Hagen, an emergency medicine nurse, has become a passionate mental health advocate since being diagnosed with bipolar disorder in her early 20s. Recently, Sally described what her behaviours and thoughts were like while manic, as well as her first experience with psychotic symptoms, which for some people can manifest as part of their mood disorder. In her article (link below), Sally shares her experiences as a way to improve our understanding of what individuals living with psychosis go through. She also encourages us to avoid holding judgment or being fearful of those affected, as often they are the ones who are terrified and confused, and require early support and treatment. "Psychosis is poorly understood by the general public and this leads sufferers to experience stigma and discrimination. Adding to the stigma, films and TV shows often misrepresent what psychosis is really like, making it something to be feared. I was guilty of not having an accurate understanding of psychosis. However, that quickly changed after my first psychotic episode. Although for a small portion of that time I may have been feared, I can guarantee I was the one who was terrified. Terrified of the unpredictable turmoil in my head, I would have harmed myself well before harming others." For the full article, click here: http://themighty.com/2016/03/what-its-really-like-to-experience-psychosis/_  New research suggests that mindful eating could not only forestall #overeating and #obesity, but #eating #disorders such as #anorexia and #bulimia as well. As a result, mindful eating practices have been incorporated into therapeutic programming at many eating disorder treatment centres. Recently, the practice of mindful eating has been integrated into schools with the hopes of decreasing the risk of eating disorder development. The #mindful #eating practice aims to teach children how to eat intuitively and to listen to their body signals to ultimately decrease risk of developing negative relationships with food. For the full article, click here: https://www.washingtonpost.com/news/to-your-health/wp/2016/03/16/how-schools-are-using-mindful-eating-to-help-prevent-eating-disorders/ New research suggests that mindful eating could not only forestall#overeating and #obesity, but #eating #disorders such as #anorexia and#bulimia as well. As a result, mindful eating practices have been incorporated into therapeutic programming at many eating disorder treatment centres. Recently, the practice of mindful eating has been integrated into schools with the hopes of decreasing the risk of eating disorder development. The #mindful #eating practice aims to teach children how to eat intuitively and to listen to their body signals to ultimately decrease risk of developing negative relationships with food.
https://www.washingtonpost.com/…/how-schools-are-using-min…/ 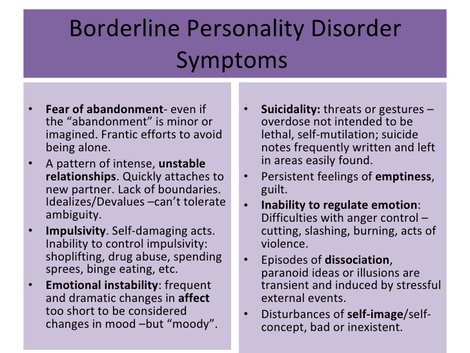 While most physicians have an understanding of the diagnostic criteria for personality disorders and can identify some of the general traits of each, our medical training often does not extend to teaching us how to disclose the diagnosis of a personality disorder to patients themselves. As a result of this, many doctors including training psychiatrists often wonder whether they even should disclose the diagnosis in the first place. In the article below, a patient with borderline personality disorder, speaks out about her experience with the mental health condition, as well as how finally receiving the diagnosis provided both her and her family with great "relief" and insight. "Having awareness of symptoms, triggers and disordered reactions is huge. I've reached the stage now where I can (in theory at least) recognise all three, although that doesn't mean the trigger or response can necessarily be avoided. Rather, I'm starting to figure out how to handle myself, what I need to do to reduce the impact of a trigger and try to avoid the most damaging behaviour. Ultimately this is where DBT will come in... Borderline is really, really hard to live with, for me, and for my family. But, clichéd and all as this may sound, it genuinely has taught us a lot. We're far more open in how we talk to each other, because communication is absolutely crucial in surviving this. The minute we stop talking is the minute problems start. Difficult conversations are all too frequent, but they have to be had. For myself, I'm increasingly aware of how other people are on an emotional level, and am far more empathic because of it. In fact, being able to identify with someone else helps me, because it takes me out of myself." For the full article, click here: http://www.independent.ie/life/health-wellbeing/mental-health/my-life-with-borderline-personality-disorder-ive-always-felt-like-an-outsider-an-imposter-someone-who-was-tolerated-34426965.html In her TEDMED talk posted just earlier this week, Dr. Pamela Wible, a family physician and self-described "specialist in physician suicide", shares stories and letters from physicians around the world all of whom have either contemplated, attempted, or died by suicide. Through these stories, Dr. Wible points to medical training and our culture of medical education as one of the culprits of the shocking numbers of physicians suffering from mental illness and suicidal ideation. Through her talk, Dr. Wible hopes to bring more light to this issue and encourage our learning institutions to bring about change in the medical classroom, so as to benefit the mental well-being of both our new physicians, as well as their future patients. "Sleep deprivation is a torture technique. Fear as a teaching tool just teaches us to be afraid. I can help doctors, though there’s one group I can’t help—patients. From all over the country they write me, begging me to find them caring doctors. How can we give them the care we’ve never received?"  Mental illness on university and college campuses has been of increasing attention recently and as a result, many schools have begun searching for ways to better support the mental well-being of their student body. One initiative that has arisen out of this is #MyDefinition, a poster and social media campaign that originated at UNB Fredericton. Through the use of photographs and personal stories from students, the campaign strives to demonstrate the wide spectrum of mental health disorders, in addition to increasing awareness of mental health on campus, and encouraging students to seek support and help by combating stigma and letting students know they are not alone. Most especially, the project also emphasizes the message that though "mental health is a part of me, it does not define me". Since it's initial development, #MyDefinition has continued to evolve and has expanded to other post-secondary schools on the east coast, including St. Thomas University (New Brunswick), Cape Breton University, and most recently Dalhousie University. "Recovery isn’t black and white. It’s not a simple classification of sick and recovered. It’s a spectrum, and a lifelong battle. It doesn’t come overnight. Every day I still battle with my mental illness. Some days I struggle to get out of bed, sometimes I dissolve into a puddle of tears when someone looks at me wrong, but those days are outnumbered by the days that are easy" - Caitlin (Dal Student). To learn more about the project and read student's stories of their own lived experiences with mental health visit: http://www.mydefinition.ca/ There is a dangerous misconception that eating disorders only affect those who physically appear as though they have an eating disorder. The fact is, eating disorders don’t discriminate, and can affect individuals of any weight, age, ethnicity, and socioeconomic class. Eating disorders can claim lives at any shape and size, so let’s ensure those who suffer receive the support and care they deserve.
http://www.washingtontimes.com/news/2016/mar/21/husband-lobbies-for-assistance-in-combating-eating/?utm_source=RSS_Feed&utm_medium=RSS  Photo by: Andrea Star Reese Photo by: Andrea Star Reese Today, the Human Rights Watch released a shocking and disturbing report regarding the treatment of thousands of individuals living in Indonesia with mental illness and related disabilities. The report, aptly titled "Living In Hell", discusses how over 18,000-19,000 Indonesians live in "pasung", a practice that involves individuals being shackled and confined and forced to eat, sleep, defecate and urine in their small cell or room. While the Human Rights Watch report that these facilities put individuals at risk of physical ailments as well as physical and sexual abuse, they also report that treatments ranging from traditional herbal concoctions and rituals to ECT without anesthesia are forced onto those who live there. Though the Indonesian government considered "pasung" inhumane and subsequently banned the use of the practice back in 1977, it continues to be utilized today. The report points to both the culturally held beliefs about mental illness, as well as an extreme lack of psychiatrists and mental healthcare facilities/services across the country as major barriers to more appropriate and humane mental health care. "Across Indonesia, there is a widespread belief that mental health conditions are the result of possession by evil spirits or the devil, having sinned, displayed immoral behavior, or lacking faith. As a result, families typically first consult faith or traditional healers and often only seek medical advice as a last resort. Even if they do look for access to medication, however, people may find it impossible to access it. Ministry of Health data shows that nearly 90 percent of those who may want to access mental health services cannot. The country of 250 million people has only 48 mental hospitals, more than half of them located in just four provinces of Indonesia’s 34 provinces. Eight provinces have no such hospitals, and three have no psychiatrists. In all of Indonesia there are just 600 to 800 psychiatrists—or one trained psychiatrist per 300,000 to 400,000 people. The few facilities and services that exist often do not respect the basic rights of people with psychosocial disabilities and contribute to the abuses against them." You can read more about the report via the video below and the following articles and photo documentation: https://www.hrw.org/node/287537 http://time.com/4265623/indonesia-mental-illness-chains-pasung-hrw/  An anonymous physician shares a deeply personal account of losing a close friend and fellow physician to suicide. While reports continue to surface of physician deaths by suicide, this story in particular has a powerful impact on readers, highlighting the stresses that can lead to physician burnout and depression, the barriers to doctors seeking help, and ultimately the impact one's death has on loved ones ... "I became good at managing the stress, though, and by this, I mean suppressing the negative feelings. Physicians are good at delayed gratification. We are good at telling ourselves we are living “normal” lives when anyone living outside of medicine would never consider our existence normal. We tell ourselves it is normal because compared to residency, it kind of is in a perverse way. It works for a while, and many are able to do it their whole careers, but some can’t. I was good at it right up until the point that I wasn’t. Being a doctor can feel very confining at times. There is an upfront investment of time and money that is greater than most professions. The “real job” often doesn’t start until your early 30s (if you have gone straight through college, medical school, and residency) and at the end of training, you have walked so far down the path it’s all you know. What if it’s not what you expected? What if you hate it? What if it’s no longer fulfilling? The chronic stress of being a physician can manifest itself as depression, anxiety, failed relationships, substance abuse or even suicide. I’ve seen all of these scenarios up close either in myself or others." For the full article, click here: http://www.kevinmd.com/blog/2016/03/many-physicians-will-lose-suicide.html |
Description
Supporting and enhancing students' and health professionals' knowledge and understanding of mental health and psychiatry
Archives
June 2017
Categories
All
|