| "Borderline Personality Disorder: The Sufferer's Experience" is an article from last March is worth a read as there is a surprising turn- the complainant with borderline personality disorder is a physician. She illustrates both the pain of living with BPD and the need for healthcare professionals to perceive it as an illness rather than a nuisance. |
|
0 Comments
 Depression has become a topic that has shifted to the forefront of discussion in recent years, partially due to it’s increasing prominence in our contemporary society, as well as the passing of celebrity figures afflicted with the illness. A study published in 2005 indicates that Major Depressive Disorder (MDD), affects 6.7% of the North American population annually, giving an indication of the somber reality of the situation. However, due to the lack of definitive quantitative assessments to diagnose the illness, a discussion still exists as to whether individuals are truly depressed. But what if it were possible to perform a test to not only help diagnose individuals and implement rehabilitation efforts earlier on, but also to offer preventative assistance to those predisposed to the illness? A new study published in Nature determined an explicit difference in specific blood biomarkers, predominantly RNA, between patients diagnosed with MDD and control patients. Furthermore, after 18 weeks of cognitive behaviour therapy (CBT), patients who had responded to the treatment and were no longer impressed showed a shift in several of their RNA transcriptional biomarkers to reflect those of the controls. Lastly, individuals who responded to the CBT showed a unique biomarker profile relative to other individuals suffering from MDD, even before the treatment began. This gives hope towards the notion of being able to not only identify individuals with MDD, but identifying which therapeutic interventions are more likely to aid them. Summary of the article here: http://www.iflscience.com/brain/blood-test-diagnoses-depression Original article here: http://www.nature.com/tp/journal/v4/n9/full/tp201466a.html Each Monday we will be learning and thinking about Global Mental Health. To get us started off, let's take a broad look at this topic. Almost 15% of the world's disease burden is attributed to mental disorders, and almost three quarters of this burden is in low and middle-income countries. Yet almost 90% of people needing access to care in these countries do not receive it. Vikram Patel is the co-director of the Centre for Global Mental Health. In this TED Talk, he speaks about the impact of this disease burden and increasing access to mental health services in developing countries. http://www.ted.com/talks/vikram_patel_mental_health_for_all_by_involving_all  Delirium is an acute state of confusion that commonly affects older adults and often goes unrecognized by health care professionals. The DSM-5 diagnostic criteria for delirium include A) a disturbance in attention and awareness; B) the disturbance develops over a short period of time (hours to days), represents a change from baseline attention and awareness, and tends to fluctuate in severity during the course of the day; C) an additional disturbance in cognition (i.e. memory deficit, disorientation, language, visuospatial ability, or perception); D) the disturbances are not better explained by another neuro-cognitive disorder and do not occur int he context of a severely reduced level of arousal (i.e. coma); E) evidence from the history, physical exam, or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substances intoxication or withdrawal, or exposure to a toxin, or is due to multiple etiologies. Would you be able to recognize the presence of delirium in a patient? To find out more about this medical emergency visit This is Not My Mom. For a brief synopsis of schizophrenia, including what it is, the basic facts about the disorder including onset, prevalence, and risk factors, as well as the common therapies utilized to aid in recovery and the key side effects to be aware of, check out the great infographic below from Global Medical Education (www.gmeded.com)!
 Physician suicide continues to be a growing topic in the news. Check out the must read article, "Why Do Doctors Have Such A High Rate of Suicide?" by Danielle Ofri, which suggests the medical environment may be at the core of the startling rates of physician suicide (1 per day in the United States). As the author eloquently describes, "medicine is a tyranny of perfection", and though the quest for perfection is one the medical culture and our healthcare systems expect, it is a goal that is often unrealistic and unattainable, and one that can lead to stress, burnout, and an array of mental health problems. "To feel that you are falling short, every day, saps the spirit of even the most dedicated of physicians. We feel as though we have been set up to fail. Even when we do manage to preserve the joy of connecting with patients and helping improve lives, the festering stress of trying to achieve the impossible takes its toll—compromised family life, drug and alcohol addictions, depression, and thoughts of suicide." 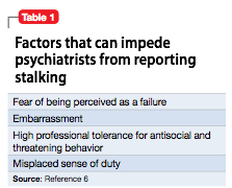 Put your knowledge and skills to the test with the case of a 48 year old female, who was previously hospitalized for persistent auditory hallucinations, and who for the last 20 months has been sending a psychiatric resident letters and postcards that total over 3000 pages. Though the resident has never treated or even interacted with the patient, the patient believes he was her physician and prescribed her medications. In her letters the patient expresses romantic feelings for the resident and "describes the resident's refusal to continue treating her as 'abandonment' and states she is contemplating self-harm because of his rejection." She goes on to threaten to strangle the resident, and threatens the resident's female acquaintances and former romantic partners which she has garnered information about from the internet. Though the resident sends her multiple requests to cease contact, they are not acknowledged, and the patient goes on to call the resident's home over 100 times for another 2 months. Can you think of how the resident can handle this situation safely and ethically? "Stalked by a 'patient'" by Jacob Appel & Stuart Kleinman (Current Psychiatry) 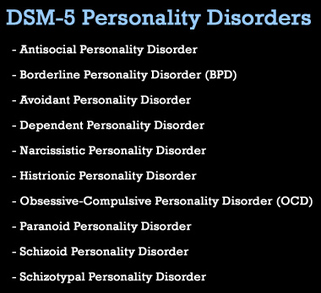 Tuesdays will now be our day to learn and reflect on personality disorders. The Canadian Mental Health Association BC division has a great page (see link below) if you are looking to become more familiar with these disorders, their causes and treatments. Stigma surrounding these disorders suggests that they are difficult to treat or even untreatable, but recent research indicates that there is reason to be optimistic. In the following weeks, we will try to focus on the experiences of individuals who deal with personality disorders in their every day lives. http://www.cmha.bc.ca/get-informed/mental-health-information/personality-disorders#personality |
Description
Supporting and enhancing students' and health professionals' knowledge and understanding of mental health and psychiatry
Archives
June 2017
Categories
All
|




 RSS Feed
RSS Feed
