
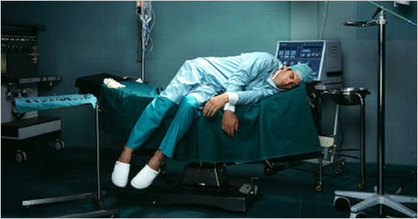
"But the fundamental barriers to well-being remain here as in other programs nationwide: our 80-hour workweeks, our massive debt-to-income ratios, and the accumulated grief of years of medical training. The first time I went to counseling was during my first month in the ER, when I had a week of day shifts, followed by a week of nights, then a week of days and then another week of nights. The therapist’s first question was about my sleep schedule—the likely cause of my distress, but also absolutely beyond my control...
...The goal of preventing physician suicide seems reasonable to me: suicide is concrete, measurable, and important. “Wellness,” on the other hand, is fishy and elusive. The duty to promote one’s own wellbeing can feel like another burden on our time, and the idea that we residents have control over our wellbeing—or much of anything in our lives—is laughable.
My residency program’s individualized learning plan survey asks us what we are doing to promote wellness. I am able to list a couple of things in the box—I walk to work, I have a husband who makes me food—but the fact is I do not believe wellness is available to me. Not in this environment, and not at 80-hour weeks."
To read the full article, visit:
"When Doctors Can't Afford to Feel" by Dr. Rachel Pearson (The Daily Beast)





 RSS Feed
RSS Feed
