
To read more about Dr. Yaffe's perspective with regard to what the movie got right (and wrong) with regard to Alzheimer's disease visit: http://time.com/3695430/how-accurate-are-health-films/item/still-alice/
 The film Still Alice starring Julianne Moore took home an Oscar last week for best actress. It chronicles the experience of Dr. Alice Howland, an accomplished professor at Columbia University, as she is diagnosed with early Alzheimer's disease. How accurately, however, does this critically acclaimed movie portray the onset and progression of this disease? Dr. Kristine Yaffe, a psychiatrist and professor at the University of California reviewed the film and offers her perspective in this interesting article recently appearing in Time Magazine. "Scientifically, the first phase of Alice's symptoms and encounter with her consultant neurologist are very realistic and deeply moving. The movie accurately demonstrates the early word-finding challenges, occasional memory lapses and sense of becoming overwhelmed in once familiar situations." To read more about Dr. Yaffe's perspective with regard to what the movie got right (and wrong) with regard to Alzheimer's disease visit: http://time.com/3695430/how-accurate-are-health-films/item/still-alice/
0 Comments
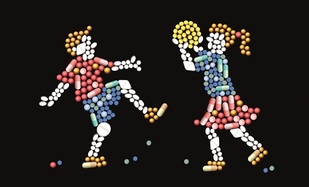 The introduction of second generation of antipsychotics in the 1990s, called “atypicals”, was hailed as a breakthrough for the treatment of schizophrenia. Only a few years later, atypicals were used for treatment of various mental diseases, including bipolar I disorder, dementia, depression, and anxiety. However, leaked documents from pharmaceutical industries reveal marketing campaigns in which scientific data were described inaccurately or suppressed and criteria for mental disorders were stretched to include a vast target range of patients. Atypical antipsychotics were promoted as treatments for conditions for which they possess a questionable risk-benefit ratio or for which there is no supporting evidence at all. To push widespread adoption of atypical antipsychotics for a wide variety of ills, the usual sales tactics were used, including: direct-to-consumer advertising (in the United States); sales visits to prescribers; touting overly optimistic cost-effectiveness research; free drug samples; sponsored medical education; peer-to-peer marketing (paying physicians to market to their peers); funding patient advocacy groups; and, perhaps most importantly, biased presentation of evidence in medical journal articles. Read more here: http://www.pharmaceutical-journal.com/opinion/comment/atypical-antipsychotics-overrated-and-overprescribed/20067929.article Did you know that recently Facebook teamed up with a number of suicide prevention organizations and research centers in hopes of helping people online prevent their friends from attempting suicide ? Beginning yesterday if a Facebook user posts a worrying status, that person’s friends can now report the post and try to get them help. The user will be contacted by Facebook and given the option to contact a Facebook friend for support, speak to a trained professional via phone or online chat, or learn about other tips and supports via an array of videos and websites. Find out more about this new feature by checking out the short video and article below! http://time.com/3723472/facebook-suicide/ Forefront FB v8 from Mimi Gan on Vimeo. A study spanning two decades, followed children into young adulthood, to determine their emotional behavioural functioning.
“Victims report the greatest anxiety problems. They might become successful people later on, but they still think about the event and hold onto it. Bullies are socially adept and may find ways in adulthood to use these skills in a pro-social manner. Folks really underestimate who are the bully-victims. These are the ones who end up having the most significant emotional problems including suicidality.” Contrary to what may have been believed in the past, that bullying is a harmless rite of passage, research is showing that the effects of bullying extend beyond the childhood years. This research lends itself as further evidence for "stop bullying" programs. Read more: http://www.nimh.nih.gov/news/science-news/2013/bullying-exerts-psychiatric-effects-into-adulthood.shtml 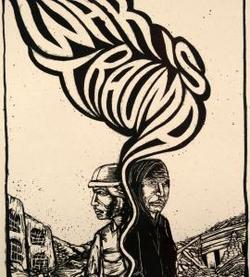 Though the role that the Canadian Forces plays and should play at home and abroad is constantly in flux, many Canadians agree that soldiering is difficult, deadly, traumatic work that deserves the support of society. Recently the Harper government issued a statement committing $200 million dollars over 6 years for the mental health of soldiers. At the same time, though, it appears that no effort has been made to increase access to mental health, counselling and rehabilitation. Worse, soldiers who are discharged prior to serving 10 years in the CF are denied pension plans that they have contributed to. The Canadian Forces requires its soldiers to serve for a period of 10 years before becoming eligible to draw upon the pension funds they contributed towards throughout their years of service. For soldiers afflicted with PTSD who are unfit to serve as a result of their illness and quit or are discharged, there is nothing available to them. No pension, no support, no new career. This issue has been covered recently by the CBC as the mental health of veterans becomes less and less stigmatized and more soldiers feel comfortable speaking out. As the CBC reported, though, '...but because they aren't eligible for a full pension before they've completed 10 years of service, many soldiers feel that coming forward with a PTSD complaint in their first decade could put them on a fast track to dismissal, says Peter Stoffer, an NDP MP and veterans affairs critic. Once the Department of Defence determines that a person has PTSD, "all of a sudden the clock starts ticking on your removal from the military," says Stoffer, who is calling for the abolishment of the 10-year rule. Based on the current rules, if Armed Forces members are released prior to the 10-year mark, they are only entitled to a return of their pension contributions.' CBC's full article on the issue can be found here. The Wounded Warrior Project, a veteran's service organization that provides services, information, programs and services for injured soldiers, can be found here.  In lieu of the Oscars taking place this evening, one of the nation's leading child and adolescent psychiatrists and founding president of The Child Mind Institute, Dr. Harold Koplewicz, speaks out about how Hollywood is making "major strides" in recognizing the importance of mental health. As Dr. Koplewicz points out, recently there has been a significant influx of films, including a few nominated for Academy Awards, that shed light on mental illness and emotional hardships that are all too prevalent today. Such movies can have a dramatic impact on the public's knowledge of mental health. Specifically, "these films can change people's minds about mental health and learning disabilities", in addition to helping end #stigma and raise awareness if they provide accurate portrayals of psychiatric disorders and psychological stress. "Mental health is often misunderstood, but it doesn't have to be. Accurate portrayals of mental illnesses such as autism or bipolar disorder in the media help the general public better understand the reality behind these diseases. One in five children copes with a psychiatric or learning disorder. Yet parents who notice signs of psychiatric or learning disorders in their children wait, on average, two years to get help for them. There are various reasons for this — parents are scared, they hope their son or daughter will outgrow it, or they think their child is just a late developer. But a major reason people hesitate to get help is because of the stigma attached to mental illness. The fact is, mental illness is real, common and treatable. That's where films like this year's Oscar nominees come in." Read more here: http://www.hollywoodreporter.com/news/top-psychiatrist-oscar-nominees-making-775536  Grief and bereavement are normal and expected human responses to the death of a loved one. What happens, however, when this grief doesn't subside? "Complicated grief is an extreme, unrelenting reaction to loss that persists for more than six months. Symptoms of complicated grief commonly include intense yearning, longing or emotional pain; frequent preoccupying, intrusive thoughts and memories of the person lost; a feeling of disbelief or inability to accept the loss; and difficulty imagining a meaningful life without that person." It is most common in women over 60 years of age and is experienced by 10-20% of widowers as is illustrated by the following case: " 68-year-old widow who continued to be seriously impaired by grief four years after her husband died. The woman slept on the couch because she could not bear to sleep in the bed she had shared with him. She found it too painful to engage in activities they used to do together. She no longer ate regular meals because preparing them was a too-distressing reminder of her loss. And she remained alternately angry with the medical staff who cared for him and with herself for not recognizing his illness earlier." To learn more about this important topic, including treatment options, check out this great article recently published in the NY Times: http://well.blogs.nytimes.com/2015/02/16/when-grief-wont-relent/?_r=0  A new approach to preventing and reducing the adverse effects of medications in people with mental illnesses will utilize personalized medicine to manage drug therapy by analyze each patient’s genetic makeup to determine potential adverse reactions to medications. This new initiative is funded by the Polk Foundation, and led by NHS Human Services in collaboration with geneticists at the University of Pittsburgh Graduate School of Public Health. “Individuals can suffer immensely from the very drugs that are meant to improve their health if given drugs they cannot tolerate, often resulting in increased emergency room visits and elevated health care costs,” said Dietrich Stephan, Ph.D., professor and chair of the Department of Human Genetics at Pitt Public Health. “The people at highest risk, such as the aged and mentally ill, often are prescribed a multitude of drugs with no insight into their genetic susceptibilities.” http://www.prweb.com/releases/2015/02/prweb12488394.htm When it comes to treatments for mental illness, often patients are provided with the options of medication and/or talk therapy. For certain individuals and for certain mental health conditions, therapy is often the standard of care, however access to these treatments can be extremely challenging. Not only are therapy services offered by the public system riddled with long wait lists and often limited to group therapy rather than one-on-one sessions due to high demand, but private therapy, while increasingly available, can be extremely expensive. The Guardian recently talked to a number of young professionals about their experiences in psychotherapy and asked for their opinions on whether they thought therapy was "worth it". You can read more about their thoughts here: "Is Therapy Worth It?" "I do find it helpful and I do find it important, but personally for me, there’s always this feeling – even when I have a great relationship with my therapist – I find it a bit strange that I have to pay someone to talk to me,” he says. “It just feels very exploitative in a way, because it’s paying for attention. It feels that way to me.” "When you are in the state of mind where you realize you might need help, you probably need it right now. And it takes a lot of time. It takes a lot of time to get an appointment. It takes a lot of time to find the right person,” she says." "With a therapist, that conversation is all about you. You get in there and you are not responsible for hurting his feelings. … With your friends, you are censoring yourself to make sure that they like you. You are censoring yourself because you know your friends’ issues and you don’t want to exacerbate their own issues that they might have." |
Description
Supporting and enhancing students' and health professionals' knowledge and understanding of mental health and psychiatry
Archives
June 2017
Categories
All
|