
 In this must read article for med students, residents and physicians alike, a surgeon describes her experience with developing burnout and depression on the job, and the immense difficulties she faced in trying to recover while working and even in taking a leave of absence from her job. More so though, the anonymous surgeon calls for all of us in the medical field to remember that we are human and that we need to care for ourselves first before we have the ability to care for our patients. "The result of burnout is depression. Mine was a deep, dark hole that sucked all the life out of me. I wanted, more than anything, to feel again — joy, sadness, anger, anything. I couldn’t look after myself. And, I certainly couldn’t look after patients. But, that was what I was forced to do. I told my chief of staff I was struggling and needed time off. They told me they would try to find a locum to cover my on-call responsibilities. But, in the meantime, I was to carry on. Despite medications, my depression continued and worsened. It was exacerbated by work... I am pleased to see the increasing awareness of physician burnout and availability of resiliency training. But, it’s not enough. It’s time to change physician work hours, so we have time to recover from the stress and emotional trauma. It’s time to trust our colleagues to look after our patients evenings and weekends when we’re not on call. And, it’s time to applaud physicians that don’t go to work when they are sick and build a system with enough human resources to fill in the gaps. Greater manpower makes it easier to fill in the gaps when those left behind aren’t already exhausted themselves. Working exhausted and stressed to a breaking point is unacceptable. It’s not just us that suffer. It’s our families, our friends, and our patients." For the full article, click here: http://www.kevinmd.com/blog/2016/01/surgeon-loves-job-killing.html We all know that stress can wreak havoc on our bodies both physically and mentally, and as such we often promote relaxation or stress-busting activities including vacations, hot baths, and exercise to ourselves, our friends and our patients. However could there be more a more effective and evidence-based relaxation intervention out there to prescribe? A new research study suggests the answer is yes. In the study, investigators from the Benson-Henry Institute for Mind Body Medicine at MGH utilized a structured relaxation and resiliency program that was then offered to individuals at a number of local hospitals. What they found was that this form of mind body training helped to significantly lower utilization of healthcare resources and services, including ED visits, lab tests and imaging, and in doing so helped to also save money. "The eight-week program, which meets weekly for about three hours, focuses on relaxation—through meditation, yoga and stress-reduction exercises—and resiliency-building, through social support, cognitive skills training and positive psychology. After the intervention, the relaxation group used 43% fewer medical services than they had in the previous year. When the researchers did a second analysis comparing the relaxation group to a control group of people with identical medical-services usage rates at the beginning, the effect was still strong: a 25% drop in clinical services." For the full story click here: http://time.com/4071897/stress-relief-healthcare-costs/ 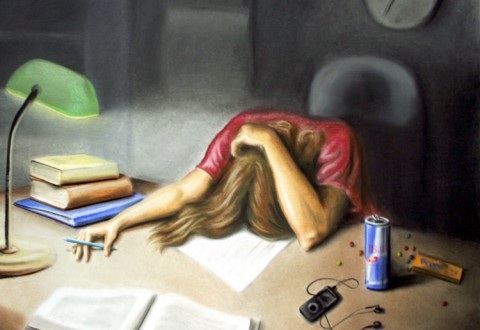 Recently on KevinMD.com, Yan Yu, a family medicine resident and Rhodes scholar from Calgary, Alberta wrote a very interesting article regarding burnout in the medical profession, and how the current culture of medical education and training may be one of the underlying culprits. More especially, using his own experiences from his med school days (which may sound all too familiar to those in the midst of clerkship), Yu explains how for many the stress and mental/physical exhaustion begins as early as medical school. It is believed that anywhere from 45-71% of med students are affected by burnout, which is "defined as the triad of emotional exhaustion, diminished sense of accomplishment, and depersonalization". Though Yu points out that burnout tends to persist into residency and beyond, and may negatively affect patient care, he also expresses that for some of us, burnout may increase our risk of suicide and mental health conditions like depression. "However, when bright, idealistic, passionate students are treated like emotionless robots, they start to become them. In the medical education community, this phenomenon is well-characterized as part of medical school’s “hidden curriculum.” By forcing students to perform menial tasks, we implicitly teach them that hospitals are not enjoyable places to learn and work. By not caring about how students feel, we teach them that getting the job done is more important than considering the feelings of others, which limits students from developing empathy for patients or compassionately treating their colleagues. Such experiences, repeated over and over, drain medical students of their energy and motivation, leaving them emotionally exhausted. Students begin to take less pride in their daily accomplishments. What was once their dream job now leaves them feeling detached and cynical. In short, they burn out – even before they become fully-qualified physicians." Read the full article here: http://www.kevinmd.com/blog/2015/09/physician-burnout-starts-in-medical-school-but-it-doesnt-have-to.html New large scale study shows that #walking recreationally to enjoy the outdoors and #nature has significant improvements in #stress reduction, mental health, and #depression. Indeed, as an affordable and accessible method of mental well being, in conjunction with the benefits of physical#exercise, it shows promise as a simple and effective modality for mind and body.
http://www.uofmhealth.org/news/archive/201409/walking-depression-and-beating-stress-outdoors-nature-group An emotional and personal #poem describing the difficulties common to the contemporary #youth, issues of eating #disorders, self image, and the veiled reassurances given to others to hide these issues.
https://www.youtube.com/watch?v=PEOFt82GMOI A simple but insightful illustration of how #PTSD is able to shape a families interactions and how it affects the extraneous relationships with other people.
https://vimeo.com/119837034 A 2015 review from Common Sense Media gives somber insight into the implications of our contemporary societies obsession with physicalappearance towards the incoming generation. Results show that an astounding 1/4 children have dieted prior to the age of 7, and that figure rises to 80% of American girls by the age of 10. A provoking read that challenges the reader to consider the repercussions of the changes we are making to combat the obesity epidemic, while concurrently aiding the issue of body image and eating disorders.
Link to the article: http://www.huffingtonpost.com/2015/01/23/most-10-year-olds-have-been-on-a-diet-_n_6532632.html Link to the original infographic:https://www.commonsensemedia.org/children-teens-body-image-media-infographic |
Description
Supporting and enhancing students' and health professionals' knowledge and understanding of mental health and psychiatry
Archives
June 2017
Categories
All
|






 RSS Feed
RSS Feed
