
 Delirium is an acute state of confusion that commonly affects older adults and often goes unrecognized by health care professionals. The DSM-5 diagnostic criteria for delirium include A) a disturbance in attention and awareness; B) the disturbance develops over a short period of time (hours to days), represents a change from baseline attention and awareness, and tends to fluctuate in severity during the course of the day; C) an additional disturbance in cognition (i.e. memory deficit, disorientation, language, visuospatial ability, or perception); D) the disturbances are not better explained by another neuro-cognitive disorder and do not occur int he context of a severely reduced level of arousal (i.e. coma); E) evidence from the history, physical exam, or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substances intoxication or withdrawal, or exposure to a toxin, or is due to multiple etiologies. Would you be able to recognize the presence of delirium in a patient? To find out more about this medical emergency visit This is Not My Mom. For a brief synopsis of schizophrenia, including what it is, the basic facts about the disorder including onset, prevalence, and risk factors, as well as the common therapies utilized to aid in recovery and the key side effects to be aware of, check out the great infographic below from Global Medical Education (www.gmeded.com)!
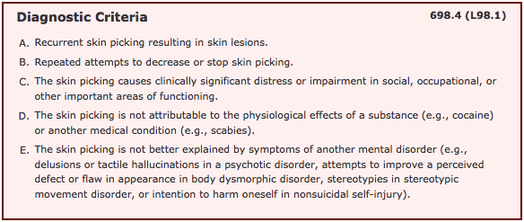
Dermatillomania, also known as excoriation disorder or skin-picking disorder, was first officially recognized as a psychiatric disorder in the most recent version of the DSM, the DSM-5. It is currently classified under the category of obsessive-compulsive and related disorders, and is "characterized by the repetitive and compulsive picking of skin, leading to tissue damage" (American Journal of Psychiatry). The face, arms and hands are the most commonly involved areas, and individuals affected with this disorder may pick/squeeze/rub/bite at healthy skin, or minor skin imperfections or lesions like acne (DSM). The onset of skin picking disorder can vary from childhood into adulthood, however for many it begins during puberty in adolescence.
 "Blackness Ever Blackening" is a descriptive and enlightening account of writer Jenny Diski's lifetime of depression, or more specifically PDD (Persistent Depressive Disorder). In her story, Diski describes her "moodiness" which began in childhood, the science and culture behind these mood disorders, her avoidance of antidepressants, and how writing has helped her. "I know that this place that I enter, the inner-space surrounding me – in which I can’t be, can’t breathe, can’t exist, but can’t not exist – also itself can’t be. A room for which there is no room. A place that makes no sense, that no sense can be made of, but which is all there is when I am in it. It is negative upon negative. Blackness ever blackening. Obscurity and obstacle always increasing, arriving at a point where nothing can be retrieved, mended – and then more and further, beyond my capacity to imagine more. A struggle that only and always resolves itself into a further impossibility, to infinity, eternity; a terrifying forever, in the most inexplicably inhuman sense of the word. And this place, this condition that has me in it, while the world mouths at me on the outside, is where I am, is what has happened, is why; and makes everything, inside and out, life itself, simply, really simply, impossible. I am islanded in the impossible, and unreachable. Yet, always the impossibility gets worse. There is no end to the worseness, the tumbling of can’tness down and down, in and in, to can’tnesses that I have never before imagined, or at any rate have forgotten, that imply further depths or intensities of can’tness that I haven’t dared to fear, but I can see coming, or me moving towards. That, roughly, is what it is like being at the blackest end of the continuum. It is like living inside this paragraph, which in its speed and insistence, melodrama and bumbling words fails to convey how awful and how physical it is, and how much I don’t want to be in it..."  For those of us who don't have autism spectrum disorder it is incredibly difficult to comprehend what life is like for someone who has an ASD diagnosis. As a result of the stigma or lack of awareness about these disorders, a number of individuals with an ASD have developed brief (1-2 minute) video simulations to help the general public gain new perspective on what it's like to have an ASD. In particular, the DSM V - Diagnostic and Statistical Manual of Mental Disorders now includes "hyper- or hyporeactivity to sensory input or unusual interests in sensory aspects of the environment" (autismspeaks.org) as part of the diagnosis, demonstrating that for many it is a core feature of the disorder. Many of the simulations that can be found at the link below highlight this sort of "sensory overload" to help us better understand what that is, as well as better appreciate and empathize with how these individuals feel and their ways of reacting or coping with such overload and resulting distress. "These sensory challenges can be very impairing, turning a normally comfortable environment into a struggle for individuals with ASD. The severity of discomfort can range widely: Anything from the cuffs of one's short-sleeve shirt to loud noises to perceptions many of us experience without thinking twice can cause distress" (mashable.com). "5 Autism Simulations To Help You Experience Sensory Overload" by Matt Petronzio (Mashable)  The Addiction Casebook is coming out next month! Find out more about it and consider adding it to your professional library. Recommended For: Medical clerks, residents and physicians in any specialty to hone their clinical skills and develop an approach to diagnosing and treating patients with substance use problems. |
Description
Supporting and enhancing students' and health professionals' knowledge and understanding of mental health and psychiatry
Archives
June 2017
Categories
All
|

 RSS Feed
RSS Feed
