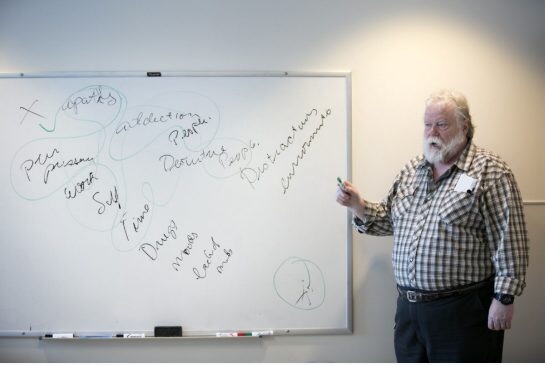
At the Concurrent Disorders Unit in Hamilton, no longer are patients kicked out if they are found to have relapsed on the substances they previously abused, nor are addictions left out of the treatment equation. Patients are not discharged until they feel ready, have learned key coping strategies, and are well connected to community supports and outpatient programs and services. On top of being the first of its kind in the country, the centre has already seen positive results in terms of relapse rates and prides themselves on cultivating a comfortable, open, and non-judgemental environment.
"IN OUR SILOED system today, addictions counsellors usually won’t work with people who are in an acute mental health crisis, and psychiatric hospitals won’t treat people who are drunk or high on narcotics.
“A typical case might be a 50-something man who is a heavy drinker and, for whatever reason, he loses his job, then his marriage and his relationship with his kids,” said Dr. Jennifer Brasch, a St. Joe’s psychiatrist who specializes in addictions.
“One night, he gets drunk and starts thinking about killing himself. If he shows up at detox, they’ll call an ambulance because he’s suicidal, and at the psychiatric hospital, they’ll dry him out. Once he’s sober, he’s no longer suicidal any more, so they’ll discharge him. But when he leaves, nothing has been solved.”
It’s a sequential approach, treating addiction before mental health or vice versa, that simply doesn’t work, Brasch said.
“It’s hard to stop drinking if you’re severely depressed. It’s hard for antidepressants to work if you’re drinking,” she said."
 RSS Feed
RSS Feed
